Migraine is a neurological disorder. It manifests as recurrent, severe headaches. These are often accompanied by other symptoms. collectively they can profoundly affect an individual's daily life. Migraine attacks typically involve pulsating or throbbing pain experienced on one side of the head. Their duration varies significantly, ranging from a mere few hours to multiple days.
Migraine Symptoms
A spectrum of experiences, unique and often challenging, characterizes the landscape for individuals affected by this neurological disorder due to varying migraine symptoms. The distinctive features that mark migraine attacks include:
Severe Headache:
Intensity and Throbbing Pain:
An intense and pulsating headache signifies a migraine. The pain typically presents as throbbing, potentially debilitating daily activities. Unlike tension headaches that may affect both sides of the head or remain centralized, migraines usually manifest on only one side. However, some individuals might encounter pain on either side.

Duration of Headache:
Several hours to days can the duration of a migraine headache last, with the pain's severity fluctuating throughout an attack. Individuals who seek effective pain management strategies must understand this crucial aspect which is the duration and intensity of these headaches.
Aura:
Visual Disturbances:
Before or during the headache phase, some migraine sufferers may experience an "aura". This manifests as visual disturbances including flashing lights, zigzag lines, and blind spots.
Other perceptual abnormalities could also be a part of these auras. Gradually developing visual symptoms act typically serve dual purposes. They indicate the impending attack of a migraine while issuing a warning signal for it.
Sensory and Motor Auras:
Auras, beyond causing visual disruptions, may also induce sensory and motor symptoms. Some people experience facial or extremity tingling, others encounter numbness. They might even confront speech difficulties or transitory paralysis.
Typically, as the migraine advances, the intensity of these symptoms diminishes until complete resolution occurs.
Sensitivity:
Photophobia (Light Sensitivity):
During an attack, many individuals suffering from migraines experience heightened sensitivity to light. This condition, known as photophobia can intensify the pain and discomfort of their headaches.
To alleviate this symptom, an often-recommended course of action involves creating a dark, quiet environment.

Phonophobia (Sound Sensitivity):
Another common feature of migraines is sensitivity to sound, known as phonophobia. Even regular sounds are not typically bothersome or loud noises can intensify discomfort related to migraines.
Olfactory Sensitivity:
During a migraine attack, some individuals may develop hypersensitivity to smells. They notice that common odors which would usually go unnoticed can trigger or exacerbate their symptoms.
Nausea and Vomiting:
Gastrointestinal Symptoms:
Frequently, migraines bring an additional layer of distress with nausea and vomiting. These symptoms can induce dehydration which is a further compromise to the individual's well-being during an attack.
Migraine Causes
To tailor effective management strategies, one must understand the multifaceted origins of migraines and the various factors that contribute to their susceptibility and onset.
- Genetic Factors:
Migraine susceptibility significantly relates to family history. If either or both parents experience migraines, their offspring may also inherit a predisposition for these headaches. Specific genetic factors might influence an individual's propensity towards migraines.
Certain genetic variations, which researchers have identified, may increase the risk of migraines. These variants could potentially sway how the brain processes pain signals and render certain individuals more susceptible to migraine attacks.
- Triggers:
In migraine prevention, it is paramount to identify and manage triggers. These are external or internal factors that can initiate or exacerbate a migraine attack. Among individuals, the variability of triggers is notable. However, some common culprits include:
- Certain Foods: Researchers have linked certain food items including chocolate, caffeine, aged cheese, and processed meats to migraine attacks in susceptible individuals.
A meticulous record of one's diet can assist in identifying specific triggers.
- Stress: Migraines are often triggered due to recognized emotional or physical stress. However, the application of stress management techniques. Specifically, meditation, deep breathing exercises, and yoga can substantially reduce their frequency and severity.
- Hormonal Changes: Particularly in women, fluctuating hormone levels can act as triggers for migraines. These often coincide with their menstrual cycle, pregnancy, or menopause. We may consider hormonal therapies to manage these specific triggers.
A dynamic process involving self-observation and professional guidance, understanding individual triggers allows individuals to identify and mitigate these factors. In doing so, they proactively reduce the occurrence of migraine attacks.
- Neurological Factors:
Fundamentally, migraines represent a neurological disorder: the brain exhibits abnormal activity and neurotransmitter imbalances. Although we have not fully comprehended the complex mechanisms involved, several key elements actively contribute to migraine pathophysiology. These are as follows:
- Cortical Spreading Depression (CSD): A wave of neuronal activity, known as CSD, traverses the brain. This movement triggers alterations in blood flow, ultimately culminating in the characteristic aura observed in certain individuals suffering from migraines.
- Serotonin Imbalance: A crucial role in regulating pain perception is played by serotonin, a neurotransmitter. The development of migraines may be a contribution from imbalances in serotonin levels.
In migraine treatment, clinicians commonly use medications such as triptans that target serotonin receptors.
- Trigeminal Nerve Activation: During migraines, the trigeminal nerve a significant pain pathway is activated. This activation contributes to the perception of pain and other associated symptoms.
Delving into these neurological factors, researchers aim to uncover more targeted treatments addressing the root causes of migraines. This pursuit paves the way for effective even personalized therapeutic approaches.
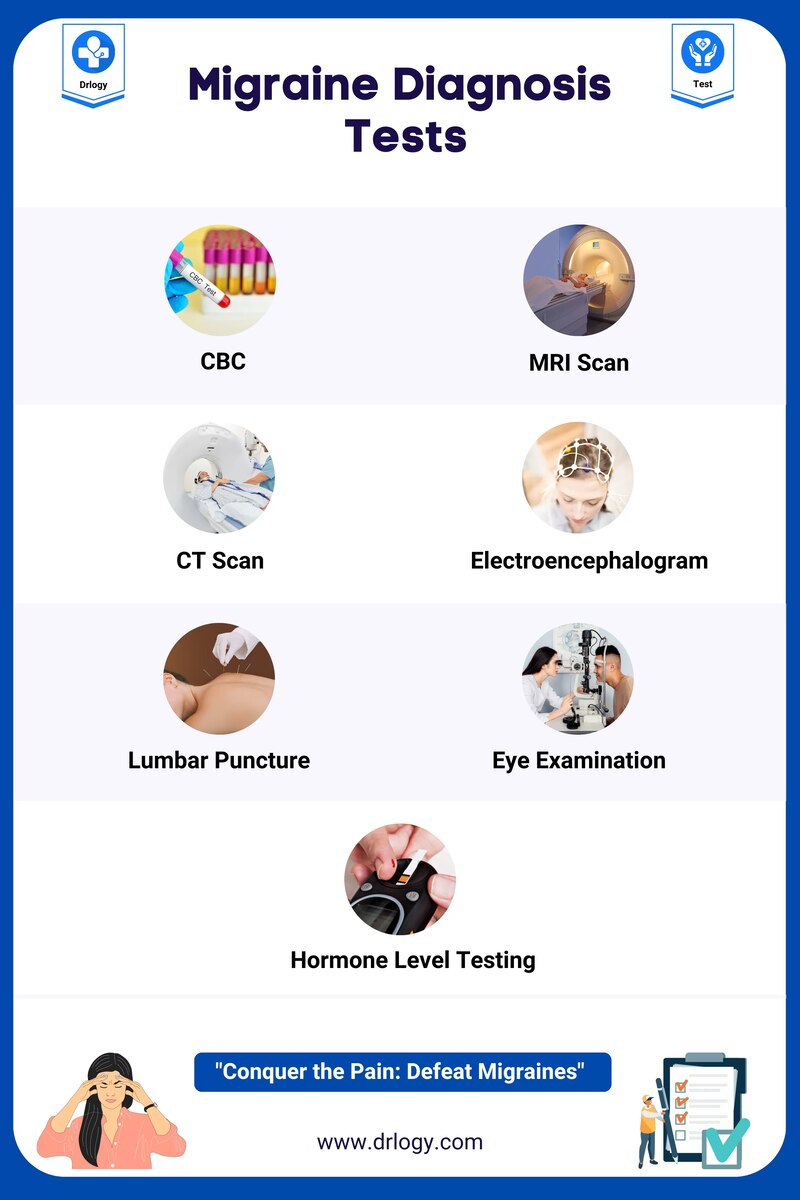
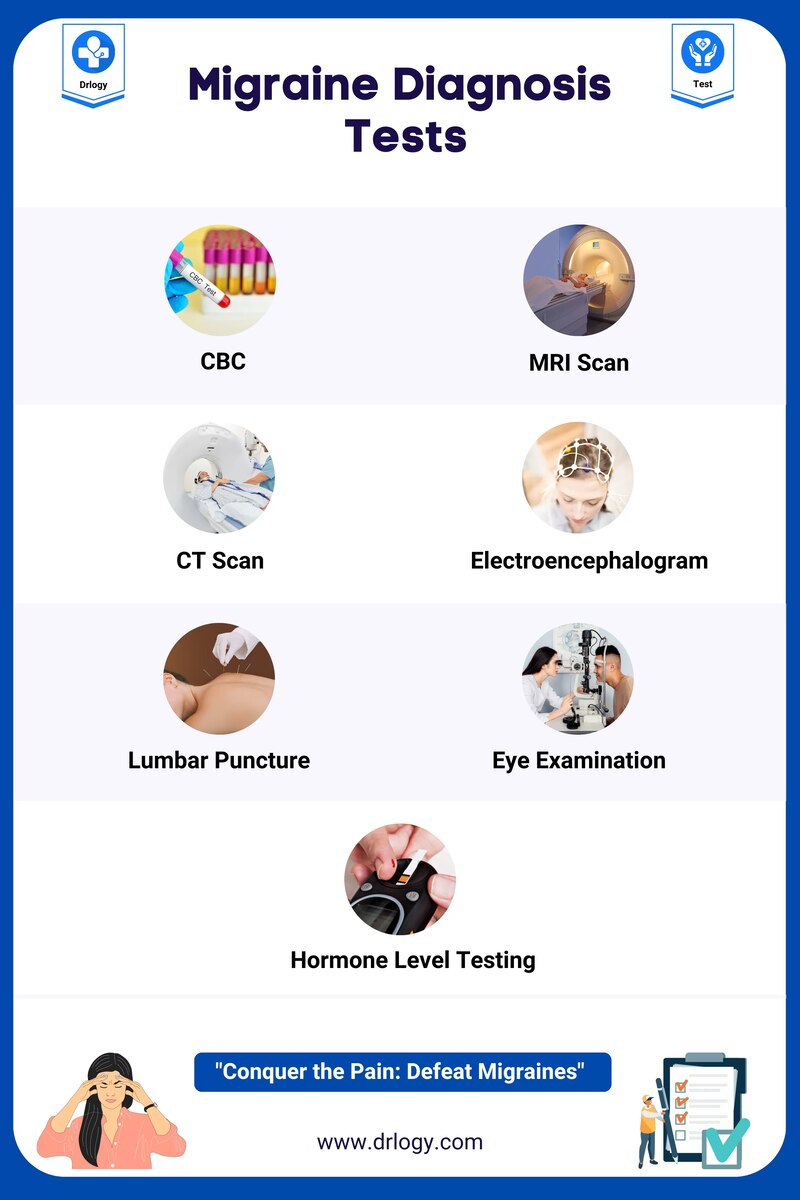
Migraine Diagnosis
Accurate diagnosis ensures proper treatment. Diagnosis involves:
- Detailed Medical History: Providing a comprehensive overview of symptoms.
- Physical Examination: Assessing neurological signs.
- Imaging Tests: MRI or CT scans to rule out other potential causes.
Migraine Treatment
A multi-faceted approach actively addresses migraines, combining acute symptom relief with preventive measures. This strategy enhances overall management.
Pain Relief Medications:
Over-the-counter (OTC) Options: People commonly use acetaminophen, ibuprofen, or aspirin (non-prescription pain relievers) to alleviate mild to moderate migraine pain. These medications function by diminishing inflammation and intercepting pain signals.
Prescription Medications: For more severe migraines, specialists may recommend prescription medications, nonsteroidal anti-inflammatory drugs (NSAIDs), or combination drugs that contain caffeine.
Triptans:
A specific class of medications, the triptans target migraine symptoms with an emphasis on relieving headache pain. By constricting blood vessels and inhibiting certain neurotransmitters' release, particularly serotonin, they play their role.
It remains crucial to acknowledge that not everyone can use triptans. Therefore, a discussion about their application with a healthcare provider is necessary, particularly for individuals presenting cardiovascular risk factors.
Preventive Medications:
Beta-Blockers: Propranolol and metoprolol are medications typically employed in the management of high blood pressure. These have demonstrated their effectiveness. Not only do they control hypertension, but also prevent migraines.
- Anticonvulsants: Prescribers can prescribe certain anticonvulsant medications, such as topiramate, to reduce the frequency and severity of migraine attacks.
- Antidepressants: Potential preventive effects on migraines may recommend the use of tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs).
- Calcium Channel Blockers: Particularly for individuals who experience aura with their migraines, one may consider medications such as verapamil.
Botox Injections:
In specific instances, specialists may administer botulinum toxin injections, commonly referred to as Botox. They target particular sites on the head and neck to prevent migraines.
We generally reserve this treatment for individuals grappling with chronic migraines. Indeed, it has demonstrated significant effectiveness, remarkably reducing their frequency.
Lifestyle Modifications:
Identifying Triggers: Identifying and circumventing personal triggers including specific foods, stress, or environmental factors can significantly contribute to preventing migraines.
- Regular Sleep Patterns: Consistently maintaining sleep patterns and guaranteeing an adequate amount of quality sleep. These are factors that actively contribute to the prevention of migraines.
- Hydration and Nutrition: Maintaining a balanced diet and optimal hydration levels. These factors can indeed have a positive impact on the frequency of migraines.
A personalized approach, considering an individual's unique characteristics and triggers, is essential for effective migraine treatment. This necessitates a collaboration with healthcare providers.
The most suitable treatment plan must be determined, balancing acute relief measures against long-term preventive strategies. To ensure its efficacy over time, regular adjustments to the plan should reflect not only on one's immediate response but also on evolving needs. It’s an interaction that underscores personalized care in managing migraines.
Prevention Strategies
To manage migraines, it is crucial to implement preventive measures. These may include but are not limited to regular exercise, maintaining a consistent sleep schedule, and avoiding triggers such as certain foods or environmental factors:
- Lifestyle Modifications: Adequate sleep, regular, balanced meals, and effective stress management. These are the fundamental pillars of maintaining optimal health. There is no compromise on their significance.
- Identifying Triggers: To minimize occurrences of migraines, one must actively avoid known triggers.
- Medication Management: Use preventive medications as prescribed consistently.
In conclusion, a comprehensive understanding of migraine includes but is not limited to an awareness of its symptoms, causes, and prevention strategies; and a grasp on the methods for diagnosis, treatment, and overall management.
By actively immersing oneself in these aspects, individuals can effectively steer their condition towards improvement. Thus, enhancing their quality of life significantly. It's important to note that consulting with healthcare professionals remains pivotal. They provide personalized guidance which is instrumental in the successful management of migraines.